A herniated disc is a common injury to the vertebrae, causing pain, muscle weakness and numbness in the limbs. If not treated promptly, a herniated disc can compress the spinal cord and nerve roots, causing many serious complications, including bowel and bladder dysfunction.
What is a herniated disc?

The disc is a “cushion” between the vertebrae, helping to reduce shock and protect the spine. It consists of two parts: a hard, fibrous outer shell and a soft, gelatinous nucleus pulposus inside.
When the fibrous outer shell ruptures, the nucleus pulposus overflows, compressing the nerves, causing pain, numbness and fatigue. This is a herniated disc, which if not treated early can lead to paralysis and affect the bowel and bladder.
Common locations of disc herniation
Disc herniation can occur anywhere on the spine, but is most common in the cervical and lumbar spine because they move the most.
- Cervical disc herniation
This condition causes pain radiating from the neck to the shoulders, arms, and hands, accompanied by numbness and muscle weakness. The cause is often due to trauma, incorrect posture, or spontaneously. However, not everyone has obvious symptoms from the beginning, so examination and X-rays are necessary for diagnosis. - Lumbar disc herniation
The lower back is under great pressure, making the disc vulnerable, causing pain radiating from the back to the legs, accompanied by numbness and decreased reflexes. Severe cases can affect bowel and bladder function, reducing quality of life.
Disc herniation rarely occurs in the chest area due to the stable structure of the thoracic vertebrae. Therefore, when mentioning disc herniation, people often think of the cervical and lumbar spine.
Progression stages of disc herniation
Disc herniation progresses slowly and is divided into 4 stages based on the degree of displacement of the nucleus pulposus relative to the annulus fibrosus
- Disc protrusion
The initial stage has vague, difficult-to-detect symptoms. The nucleus pulposus only changes slightly but is still located within the annulus fibrosus. - Prolapsed disc
The annulus fibrosus is weakened, the nucleus pulposus is pushed out to form a bulge but has not completely escaped thanks to the outermost fibrous layer that still maintains its strength. - True disc herniation (Disc extrusion)
The annulus fibrosus is torn, the nucleus pulposus spills out, compressing the nerve, causing pain, numbness or tingling. - Sequestered disc
The nucleus pulposus separates into small pieces, compressing the nerve root or falling into the spinal canal, causing severe pain, muscle atrophy, and loss of urinary control. This is a dangerous stage, often requiring surgery.
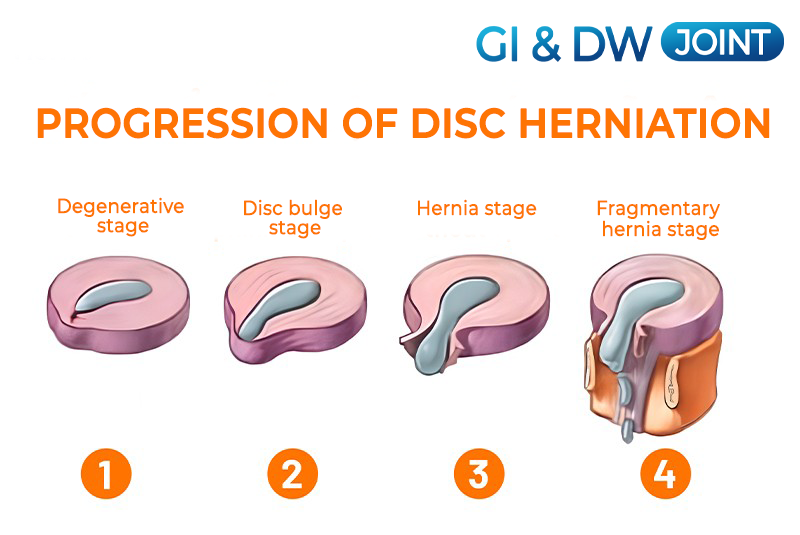
If detected early in the first two stages, the chance of recovery is very high. Therefore, early recognition of symptoms is the key to effective treatment.
Signs of a herniated disc
Symptoms of a herniated disc often appear on one side of the body, depending on the location and level of nerve compression. Some early signs include
- Pain
Pain is a typical sign of a herniated disc. If it occurs in the neck, you will have pain in the neck and arms. If it occurs in the lower back, the pain spreads to the buttocks, thighs, calves and feet. The pain increases when coughing, sneezing or moving, often with a burning sensation. - Numbness and tingling
Numbness or tingling occurs in the area of the body where the nerve is compressed. This symptom appears early on but is often overlooked. - Muscle weakness
Damaged nerves weaken the muscles, making you more likely to stumble, reducing your ability to grip and support.
Symptoms of disc herniation are easily confused with other diseases, so a visit to a reputable medical facility is necessary for accurate diagnosis and timely treatment.
Causes of disc herniation
The causes of disc herniation vary from person to person, but are mainly due to two main factors:
- Damage to the spine
Incorrect posture, carrying heavy loads, sudden changes in posture or overwork can damage the spine. When the spine is affected, the discs – the supporting parts between the vertebrae – cannot avoid damage. - Natural aging
Over time, the discs lose water, become less flexible and tear easily even with light impact. Degeneration of the spine also increases pressure on the discs, making herniation more likely.
In addition, some factors that increase the risk of disc herniation include:
Weight: Being overweight increases pressure on the discs, especially in the lumbar region.
Occupation: Porters, construction workers, people who sit or stand for long periods of time (mechanics, hairdressers, factory workers, etc.) are at higher risk.
Genetics: People with a family history of disc herniation are more susceptible to the disease.
Smoking: Smoking reduces the oxygen supply to the disc, accelerating the aging process.
Driving frequently: Sitting for long periods of time and the vibrations from the vehicle have a great impact on the spine.
Lack of exercise: Exercise helps the disc absorb nutrients, so lack of exercise can increase the risk of herniation.
Disc herniation can be caused by one or a combination of causes, and is not limited to any age or occupation.
People who are more likely to get a herniated disc

There are certain people who are more likely to get a herniated disc, including:
- People who exercise regularly and have gained weight.
- People who have muscle or joint problems and are taking painkillers such as steroids, which increase the activity of joint plasticizers.
- People with a family history of herniated discs.
- People who work in jobs that require great strength or standing for long periods of time.
- People who are older, because the body’s ability to heal itself and become more flexible as we age.
- However, a herniated disc can also occur in anyone, regardless of age and initial health status. Other causes that can cause this condition include:
- A stroke or accident that causes abnormality or pressure on the joints and discs.
- An imbalance in muscle activity can cause the condition.
- The decline in the body’s and joints’ ability to repair themselves as we age can also increase our risk of disease.

Proven effectiveness of GI JOINT & DW JOINT
Survey results show:
- 98% of users are satisfied with the effectiveness of GI JOINT & DW JOINT.
- 76% of customers feel very satisfied after use.
Subjects of use and dosage of GI JOINT & DW JOINT.
Target audience
With ingredients of safe and benign origin, GI JOINT & DW JOINT almost does not cause side effects to the liver, kidney, stomach, does not destroy internal organs and does not cause increase or decrease in blood pressure. It can be said that GI JOINT & DW JOINT brings long-term, sustainable effects to patients. According to research, GI JOINT & DW JOINT joint pills respond well to the following cases:
- Osteoarthritis, spondylosis, disc herniation, spinal calcification.
- For people with aching joints, back pain, neck and shoulder pain, swollen joints, numbness in limbs due to osteoarthritis.
- Very good for both spinal pain, degeneration in joints and limbs.








